Pressure sores affect 700,000 people in the UK each year, with 180,000 of these being newly acquired injuries.
In 2015-16, treating pressure damage cost the NHS more than £3.8 million every day.
These alarming statistics show that the importance of correct pressure care management cannot be overlooked.
Little wonder then, that NHS England have described managing pressure injuries & preventing their development as a “priority for policy makers, managers & practitioners alike”.
With this in mind, let’s look at the definitions, symptoms, grading and treatments of pressure sores.
Jump straight to…
What Are Pressure Sores?
Pressure sores (or decubitus ulcers) are injuries to areas of the skin that have been placed under pressure because a person is unable to move or change position.
They usually develop over time but can sometimes form in just a couple of hours.
There has been some commentary over the correct terminology that should be used; the traditional term was bed sores but this has been sidelined in favour of pressure injuries or pressure ulcers.
All these terms are interchangeable, and in our view it doesn’t really matter which one is used – the main thing is we raise awareness of the issue, open up the conversations and work on solutions, because this is a massive issue across the healthcare industry and one that we are passionate about resolving.
Why Do They Develop?
Pressure sores develop when pressure is applied to part of the skin and cuts off the blood supply. They can lead to breakdown in the surface of the skin (the epidermis) and, in more serious instances, the tissue beneath the skin (the dermis).
In the most severe cases, pressure ulcers can lead to the skin and underlying tissue in the affected area eventually dying.
Moisture on the skin can also increase the chances of a sore developing, and the elderly and those in low mobility scenarios are more at risk.
From acute care settings to community and residential care, any situation where patients can be sat or laid on inadequate surfaces for prolonged periods of time is one where pressure ulcers are likely to develop.
Sitting, sleeping or lying on the correct type of surface decreases the chances of developing pressure injuries, and can even manage existing sores as well as preventing them from becoming more severe.
Find A Chair That Won't Cause Pressure Sores
What Are the Symptoms of Pressure Sores?
Symptoms of pressure ulcers can include swelling and changes in skin colour, warmth, tenderness, and pain in the affected area.
A pressure injury has begun to form if pressure is removed from the affected area and the skin doesn’t return to normal after 10-30 minutes. This is referred to as a non-blanchable erythema, in other words the skin doesn’t ‘blanche’ and return to its normal colour tone after the applied pressure is removed.
People with white skin tend to get red patches, while these same pressure ulcers tend to be purple or blue on people with dark skin.
If untreated, skin may crack and leave an individual very susceptible to infection.
Who is at Risk of Pressure Sores?
Pressure injuries can happen to anyone that is sat or laid down for a prolonged period of time. They are more common in people with low mobility who spend lots of time in a chair or bed.
Older adults are the most likely to develop a pressure ulcer, one reason for this is that hospital admission generally increases the chances of them developing.
The incidence of pressure ulcers in hospitals amongst inpatients is 3-14%, this can be as high as 70% in patients with orthopaedic problems.
It is incredibly important that proper pressure care is practiced, not only to avoid worsening of a pressure injury, but to reduce the likelihood of a patient being hospitalised.
Pressure ulceration in elderly patients is associated with a fivefold increase in mortality.
This means that, particularly for the elderly, any illness that may increase the chances of being hospitalised also increases the likelihood of developing a pressure ulcer because of hospitalisation.
How Common are Pressure Sores?
In the UK, just under half a million people will develop at least one pressure ulcer in any given year.
Pressure injuries are most common in people with underlying health conditions as this is who is most likely to spend long periods of time in a hospital bed or wheelchair.
Around 1 in 20 people that are admitted to a hospital with a sudden illness will develop a pressure ulcer.
People over 70 are the most vulnerable as they are likely to have low mobility and ageing skin, this group is also very likely to be hospitalised.
Can Pressure Sores get Worse?
Yes, pressure injuries can worsen and even become life threatening if not properly treated. Due to the ease in which these sores can be infected, it is of paramount importance that proper wound treatment is practiced.
Proper nutrition, consistent wound treatment and regularly offloading pressure from the affected area can help prevent the worst outcomes.
What is a Sacral Pressure Sore?
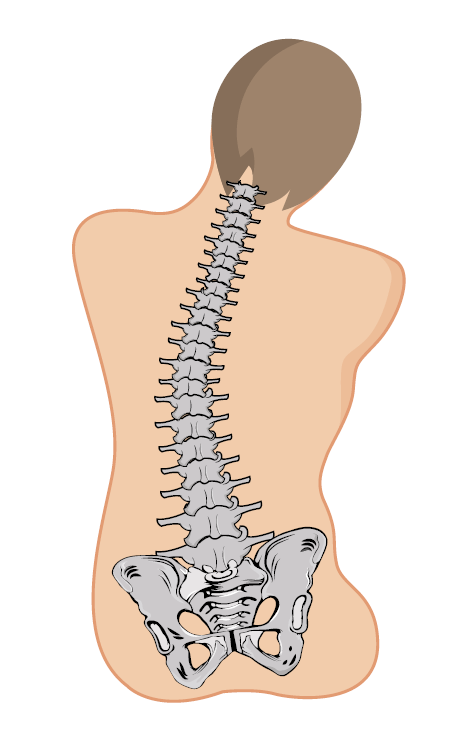
Sacral pressure sores are a very common type of injury, this refers to a pressure injury that occurs in the sacrum which lies between the fifth segment of the lumbar spine and the coccyx.
Sacral pressure is what most people have experienced when sitting on a hard surface for a long period.
Sacral sores are common, because sores tend to form on the areas of skin covering bony areas of the body such as the:
- Buttocks
- Back
- Tailbone
- Hips
- Elbows
- Heels
- Ankles
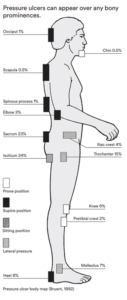
Skin over bony prominences is where someone is most likely to develop pressure ulcers, so these areas require the most protection.
Need A Chair With Pressure Relief?
Pressure or Bed Sore Grading
When pressure ulcers occur and damage the skin, they can do so at varying levels depending on how long an individual has been confined the position that caused the ulcers.
The severity of pressure ulcers is measured on a grading scale (Grade 1 — 4), with grade 4 being the most serious.
Grade 1
- Non blanchable erythema
- Skin discolouration, usually red on light-toned skin or purple/black if more severe
- Blueish/purple on darker toned skin.
Grade 2
- Partial thickness skin loss
- Skin damage or loss involving the top skin layers
Grade 3
- Full thickness skin loss
- Necrosis (death) of the skin and its underlying layers, exposing the fat layer (orangey yellow in colour)
Grade 4
- Full thickness tissue loss right down to the bone
- Exposes muscles, bones, and tendons to infection
Grade 3 and Grade 4 bedsores are almost like an open door for bacteria and infection. It is very important that this level of injury is treated immediately by a medical professional.
Deep Tissue Injury
A Deep Tissue Injury (DTI) is a type of tissue damage that is slightly different to a pressure ulcer.
Pressure ulcers usually come with a breakage of the skin, but a deep tissue injury is not always associated with broken skin and can therefore be harder to identify. They are caused by subcutaneous tissue deformation, where the tissue beneath the skin surface becomes deformed or squeezed by pressure between a bony prominence and the sitting/lying surface.
The European Pressure Ulcer Advisory Panel (NPUAP) updated their definition of pressure injuries in 2007 to include DTIs.
Unstageable
- Ulcer that has full thickness tissue loss but is either covered by extensive dead necrotic (dead) tissue or by an eschar.
- The base of the ulcer is covered by slough (yellow, tan, grey, green or brown)
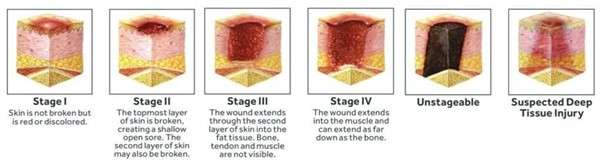
Pressure ulcer stages
Mucosal Membrane Pressure Injury
This is a type of pressure injury that occurs when pressure is applied to a ‘mucous membrane’.
Mucous membrane is a moist lining in tracts & passages in the body like the nasal passages, gastrointestinal & urinary tracts. When pressure is applied to this tissue, it can lead to ulcers developing. These tissues are vulnerable to pressure from medical devices like oxygen tubes and catheters.
Because of this, Mucosal Pressure Ulcers (MPrU) are pressure ulcers found on mucous membranes with a history of a medical device in use at the location of the ulcer.
Don't Put Up With Pressure Ulcers
Can Pressure Sores be Treated?
Yes, treatment is possible, but is also dependent on the severity. Experts strongly believe that bedsores shouldn’t ever get past the first stage. What adds particular weight to this is that the structure of the skin never full recovers after a pressure sore, when you compare the skin on a healed sore to the neat criss-cross lines on healthy skin tissue.
Low grade (stage 1 & 2) pressure injuries can be treated and usually require basic nursing care.
Stage 1 can take a few days to a week to heal with proper care, including relieving pressure on the affected area.
Stage 2 can be 1 to 3 weeks, with treatment such as cleaning the wound, keeping it moist, and relieving pressure.
Medium to high grade (stage 3 & 4) can be extremely serious, leaving a person susceptible to infections and can cause life-threatening complications.
Stage 3 pressure ulcers can take 1 to 4 months to heal, depending on the extent of tissue damage and the care provided.
Healing of Stage 4 ulcers can be very slow, and can take anywhere between 3 months and 2 years, often requiring specialised wound care or even surgery.
Severe pressure injuries (stage 3 or 4) may never fully heal in some cases, especially in individuals with limited mobility or other health complications, which is why early intervention and prevention is so critical.
Treating unstageable pressure injuries is a longer process, the pressure wound is first put through a debridement process where the wound is cleaned, and infected tissue and other debris is removed. Debridement is done so that the wound can be properly staged and treated.
How to Treat Pressure Sores
There are various treatment methods available for multiple stages of pressure injuries and the correct treatment method varies depending on the seriousness of the ulcer.
- Relieve pressure through regular movement and position changes
- Apply dressings that speed up the healing process
- Bandaging with gauze or foam
- Use specially designed static foam mattresses or cushions
- Use dynamic mattresses and cushions that pump a constant flow of air
- A procedure to clean the wound and remove the damaged tissue (debridement)
Dressings
Various dressings are available as treatment for pressure ulcers, they can be used to protect pressure injuries and speed up the healing process.
Alginate dressings — this type of dressing is made from seaweed and contains sodium & calcium which are both known to speed up the healing process
Hydrocolloid dressings — this type of dressing contains a gel that encourages growth of new skin cells in the ulcer and keeps the surrounding skin healthy
Other dressings — these can be foams, film, hydrofibres/gelling fibres, gels, and antimicrobial (antibiotic) dressings.
Pressure Cushions & Mattresses
Using the right cushioning on beds and chairs can relieve or prevent pressure ulcers.
A pressure cushion for a chair can come in a simple square or rectangular shape, or as a wedge to place on your regular seating area.
A pressure mattress acts in the same way but for the entire body, they are filled with a combination or foam, gel and air cells to relieve pressure on areas of the skin.

Airflow mattress
Take a look at our beds & mattresses range for pressure care management, with options to care for low-grade pressure injuries as well as high-grade sores that require more specialist attention.
Moisture Barrier Cream
This is a cream that protects the skin’s exposure to moisture, urine & stool. Moisture increases the likelihood of a pressure ulcer forming and a barrier cream reduces the risk of this happening.
Antibiotics
For the highest grades of pressure injuries, antibiotics may be prescribed to treat an infected ulcer. These infections can be:
- Blood poisoning — also known as sepsis
- Bacterial infection — known as cellulitis
- Infected bone — osteomyelitis
Diet & Nutrition
Diet & nutrition will not stop pressure injuries from developing if you are resting on imperfect surfaces, but a diet containing a good amount of protein and a variety of vitamins & minerals will help speed up the healing process. It is also important to stay well hydrated, as dehydration can slow down the healing process.
Summary
The legendary public health figure Florence Nightingale once said, “If the patient has a bedsore, it’s generally not the fault of the disease but of nursing”.
This view is echoed by today’s pressure care experts who believe that pressure sores can be avoided with proper procedure, and recommend that skin assessments for patients at risk of pressure ulcers should be completed at least once a day.
The problem of pressure injuries has increased in modern times as people live for longer and obesity increases, but they are highly preventable, therefore healthcare professionals must use the correct equipment and strive to give patients proper care.
Take a look at our specialist seating & range of care beds & mattresses to see how our products could offer you the pressure injury management that you need.
Alternatively contact us and talk to one of our expert seating specialists who will guide you through our range, ensuring we find the right seating for managing pressure injuries.
Get Expert Advice
FAQs
What are the typical symptoms of pressure sores?
Common signs include skin discoloration, swelling, tenderness, and pain. Advanced sores may lead to cracked skin and infection.
How are pressure sores graded?
Pressure sores are categorised into four grades based on severity, ranging from discoloured skin (Grade 1) to exposed bone (Grade 4).
Grade 1— Skin discolouration
Grade 2 — Partial thickness skin loss
Grade 3 — Full thickness skin loss
Grade 4 — Full thickness tissue loss
Can pressure sores be treated?
Yes, treatment options include repositioning, specialised cushions and seating, wound care, and in severe cases, debridement and antibiotics.
How long do pressure sores take to heal?
The healing time for pressure sores (also called pressure ulcers or decubitus ulcers) depends on several factors, including the severity of the sore (categorised into stages), the individual’s overall health, and the quality of care received.
Let's Get You Comfortable