In this article we consider the following patient scenario:
“My 88-year-old husband is bedbound but hoisted to a riser recliner chair. What is the maximum period for him to be in the chair?”
Taking care of a bedbound loved one requires balancing their comfort and health. For individuals who rely on a hoist to transfer to a riser recliner chair, it’s essential to consider how long they can remain in the chair without compromising their well-being and additional risks such as development of pressure ulceration. This article provides guidance on the maximum recommended duration for chair use and crucial steps to prevent pressure ulcers.
Jump straight to...
Maximum Time in a Riser Recliner Chair
The specific amount of time an 88-year-old bedbound individual can spend in a riser recliner chair varies depending on their physical condition, skin integrity, and overall health. Remaining seated for extended periods of time increases the risk of pressure ulcer development over the buttocks, as the soft tissue in this area is squashed between two surfaces, the chair seat and the bones.
How long will it take for pressure damage to occur? We know from contemporary understanding of pressure ulcer development it can start to occur quickly in some individuals before any visible signs on the skin surface1. Health professionals use risk assessment tools such as Purpose T2, which take into account a person’s range of independent movement, health conditions and nutritional status to form an indicator on level of risk that can lead to skin breakdown. For those who are at risk of pressure ulcers developing, tilt-in space, recline and elevating leg rests in wheelchairs and chairs are sometimes useful in providing pressure relief3,4.
However, as a general guideline:
- Does the person have any ability to change position, and maintaining an upright-seated position without slumping or sliding which can cause shear forces related to pressure damage
- Pressure relief should be performed every 30 minutes lasting 30 seconds5
- Individuals should not remain seated for longer than a 2-hour period at any one time during the day6
- If sitting in a chair is necessary for individuals with existing pressure ulcers in the seated region, sitting should be limited to three times a day in periods of 60 minutes or less. The individual’s seat, posture and sitting times should be reviewed and modified if the pressure ulcer fails to improve7
- Pressure and or shearing of the skin over this period can become starved of oxygen and essential nutrients causing cells to die and pressure ulcer formation
Always consult with a healthcare professional, such as a nurse or physiotherapist, who can provide tailored advice based on the individual’s specific needs and medical history.

Pressure-Relieving Equipment
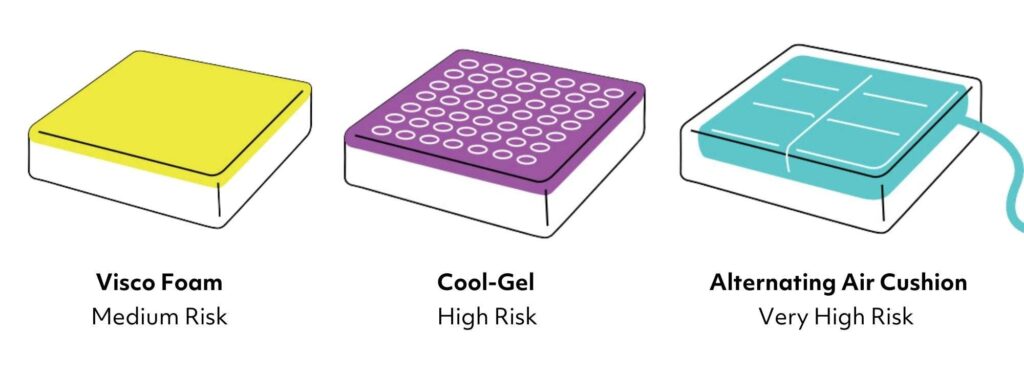
- There are many different types of pressure redistributing seating equipment available to help prevent and manage pressure ulcers.
- Static cushions and pressure seating built into chairs such as those made using foam, gel, and air are made to decrease the risk of tissue damage by redistributing pressure at the bony points in the pelvic area of the seated individual.
- Particular attention should be paid to reducing the pressure exerted on the areas at risk, managing temperature and humidity at the buttocks, and comfort.
- Check the seating area and cushion for any objects and do not cover pressure relief cushion with sheets or blankets which can reduce the effectiveness of the equipment.

Signs and Symptoms of Pressure Damage
Look for changes in a person’s usual skin colour particularly in areas where the bones are beneath such as: the buttocks, lower back and spine, shoulder blades, hips, back of the knees, heels and elbows.

90 degree sitting angle
In light skin tones the area may appear pink or red which does not go away when pressing on it with a finger. In dark skin tones, the area may appear blue or purple. Also consider how the skin feels, harder or softer and temperature changes, heat and cooler.
Do these signs resolve when the pressure is taken away from this area by repositioning? If not, seek advice and support from a professional.
Importance of Repositioning
Even when seated in a supportive riser recliner chair, prolonged periods in one position can lead to pressure ulcers (also known as bedsores). These injuries develop when prolonged pressure reduces blood flow to the skin and underlying tissues, particularly over bony areas such as the tailbone, hips, and heels.
To mitigate this risk:
- Reposition the individual regularly even if only slightly adjusting their posture.
- Use specialised cushions or chairs designed to redistribute pressure when seated.
- Encourage gentle movements or stretches, if possible, to stimulate circulation.
- If possible and able and safe, movement may be performed using the “roll” (a side-ways lean); a “forward lean” where the individual leans forward with their chest over their thighs, and can be effective at reducing pressure underneath the ischial tuberosities8
- Moving and handling equipment such as slings are not left under the buttocks when transfers have occurred
Pressure Ulcer Prevention Tips
Preventing pressure ulcers requires a proactive approach. Here are some best practices:
Skin Care Routine
- Inspect the skin at least once daily for early signs of pressure damage.
- Be mindful if any medical devices are in place such as catheters which can also cause device-related pressure ulcers. Ensure they are secured comfortable.
- Ensure continence regimes are in place and if pads are used, fitted correctly reducing moisture-associated skin damage risk.
- Keep the skin clean and dry. Use PH balanced skin cleansing and moisturisers to maintain skin integrity.
Nutrition and Hydration
- Ensure a balanced diet rich in vitamins and protein to support skin health and tissue repair.
- Encourage adequate fluid intake to keep the skin hydrated and resilient.
- If restrictions inhibit intake, seek support and advice from health professionals.
Regular Monitoring and Professional Support
- Ensure healthcare professionals are involved to aid in assessment and guidance.
- Education for family and carers is essential to enable supported self-care.
- Seek immediate advice if you notice any early signs of pressure ulcers.
Creating a Comfortable and Safe Environment
Seating assessment should be person-centred. The individual needs to understand why specialist equipment is required, the potential impact on their lifestyle and benefits such as the prevention of pressure ulcers9. Comfort is key to enhancing quality of life. Ensure that the riser recliner chair is appropriately adjusted to support their posture, with head, back, and leg supports tailored to their needs. Care must be taken with recline features which can lead to sliding and exacerbate pressure and shear forces if the person is not positioned correctly in the chair. Sliding/slipping from the chair with the riser feature is a risk if operating the chair alone.
Final Thoughts
Comfort and postural stability, pressure redistribution, physiological abilities e.g. breathing, swallowing, digestion, participation in occupations and activities such as hobbies and daily living tasks all impact on the person’s quality of life and communication10.
References:
- Ref Gefen A, Brienza DM, Cuddigan J, Haesler E, Kottner J. Our contemporary understanding of the aetiology of pressure ulcers/pressure injuries. Int Wound J. 2022 Mar;19(3):692-704
- Coleman S, Smith IL, McGinnis E, Keen J (2018) Clinical evaluation of a new pressure ulcer risk assessment instrument, the pressure ulcer risk primary or secondary evaluation tool (PURPOSE T). J Adv Nurs 74(2):407–24
- RESNA position on the application of tilt, recline, and elevating leg rests for wheelchairs. 2008. Retrieved from “RESNA Position on the Application of Tilt, Recline, and Elevating Legrests for Wheelchairs” document.
- Stinson MD, Porter-Armstrong A, Eakin P. Seat-interface pressure: a pilot study of the relationship to gender, body mass index, and seating position. Arch Phys Med Rehabil 2003;84(3):405e9.
- Sonenblum S, Vonk T, Janssen T et al (2014) Effects of wheelchair cushions and pressure relief manoeuvres on ischial pressure and blood flow in people with spinal cord injury. Arch Phys Med Rehabil 95(7): 1350–7
- National Institute of Health and Care Excellence. Pressure ulcers: prevention and management. 2014. Retrieved 19/01/16 from, http://www.nice.org.uk/ guidance/cg179/chapter/1-recommendations.
- National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance (2014) Prevention and Treatment of Pressure Ulcers: Quick Reference Guide. Available online at: https://www.npuap.org/wp content/uploads/2014/08/Updated-10-16-14-Quick-Reference-Guide-DIGITAL NPUAP-EPUAP-PPPIA-16Oct2014.pdf {accessed 08/05/2025}
- Stockon L, Gebhardt K and Clark M (2009) Seating and pressure ulcers: Clinical practice guidelines. J Tissue Viability 18(4): 98–108
- Stephens M and Bartley C (2018) Understanding the association between pressure ulcers and sitting in adults what does it mean for me and my carers? Seating guidelines for people, carers and health & social care professionals. J Tissue Viability 27(1): 59–73
- AWTVNF, PUPIS. All Wales Best Practice Guidelines: Seating and Pressure Ulcers. London: Wounds UK, 2019














