Pressure ulcers, also known as bed sores or decubitus ulcers, are a serious healthcare concern worldwide. International awareness campaigns such as “Stop Pressure Ulcer Day” highlight the need for better wound care strategies in healthcare. Every year, the EPUAP marks Stop Pressure Ulcer Day on the third Thursday in November to call for change and raise the profile of this global issue.
In this article, we explore effective methods to prevent pressure ulcers, offering practical care plans for healthcare staff and solutions for systemic change.
Jump straight to...
Person-Centred Strategies for Pressure Ulcer Prevention
When delivering personal care in patient settings, there are processes and equipment that can guard against the risk of pressure ulcers. A combination of using the right equipment with the right care plan and techniques can dramatically reduce the risk of pressure wounds.
Risk Assessments
It is everyone’s job in healthcare to prevent pressure ulcers developing. There are some simple wound care strategies that can be employed by ward staff and carers, but it needs the awareness of all staff and initiative of senior management to implement these strategies effectively.
Risk assessments are a powerful tool to mitigate risk and check off against a pre-planned checklist in a consistent way.
1. SSKIN
“SSKIN” is the standard criteria used to guard against pressure sores generally.
| Surface | Make sure the surface they are sitting/lying on provides the right pressure relief, see more on this below |
| Skin | Check the skin for pressure sores forming, in the early stages these are characterised by blanching (red turning to white when pressed with a finger) |
| Keep | Keep the patient moving |
| Incontinence | Moisture helps pressure sores develop, so ensure the patient is kept clean and dry |
| Nutrition/Hydration | Make sure your patient is on the right diet and drinking plenty of fluids, as obesity is a factor in pressure sores |
2. Braden Risk Assessment Tool
The Braden Risk assessment tool combines the features above into a rating mechanism to assess the degree of risk. Individuals with a total score of 16 or less are considered at risk.
Seat Fabrics and Systems
Seat fabrics and materials can go a long way in reducing the build-up of pressure. Particularly for patients who are not able to reposition themselves easily, having the right pressure relief built into the chair is an essential feature.
1. Vinyl
Vinyl is a hard-wearing and bacteria-resistant fabric, but not as good for pressure relief. A vapour-permeable fabric like dartex is best for contact surfaces, as it is soft, stretchy and water-repellent, preventing the build-up of moisture and keeping the skin cool and hydrated.
2. Dartex
Dartex is a good fabric combination with pressure relieving foam or gel, as it doesn’t compromise the pressure relieving qualities of the upholstery underneath. Medium or high risk foam can be specified, with gel inserts if required, to relieve pressure on bony areas.

Lento care chair with dartex fabric
3. Alternating Air Systems
Alternating air systems, found in pressure relief mattresses, can also be built into care chairs if required. They have alternating soft and hard air cells which change every 10 minutes or so, preventing the build-up of pressure.
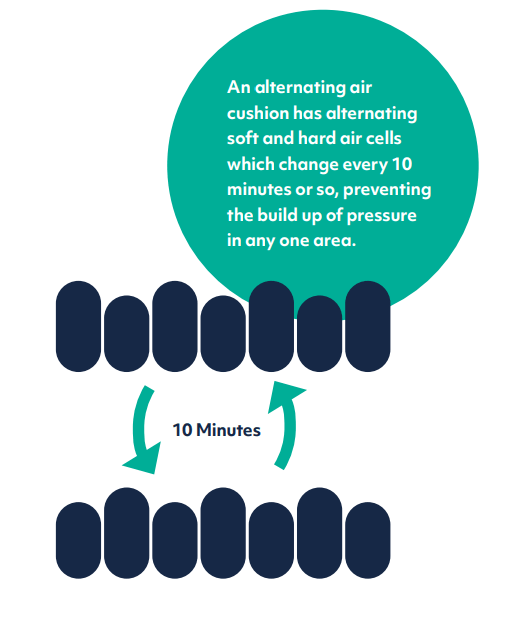
Alternating Air system
Tilt In Space
This is an integral feature for assistive chairs, as it redistributes pressure over a wider surface area of the body. The patient is rocked back in the chair while keeping the same hip angle. With dual motor tilt in space, the backrest and legrest can be adjusted independently to improve postural positioning even further. This simple action reduces pressure on the buttocks and thighs, spreading it more evenly over the body to alleviate build-up in one area.
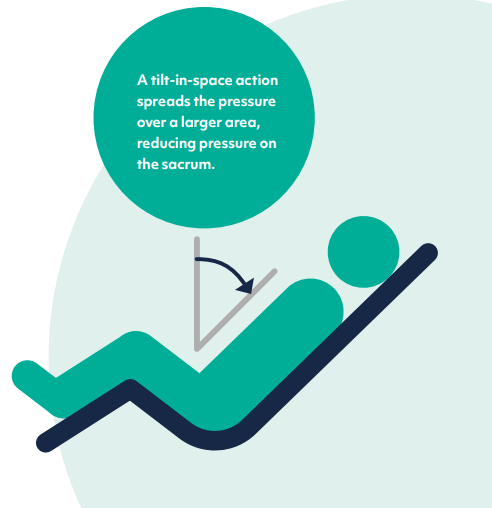
Tilt-in-space functionality
Pressure Mapping
Pressure mapping is a visual representation of the distribution of pressure on a particular area of the body. Pressure mats can be used on a patient’s seat or mattress and linked to a monitor, showing the degree of pressure on different points. This is particularly useful as a ‘before and after’ tool, to see the effect of incorporating extra pressure-relieving materials into a bed or chair.
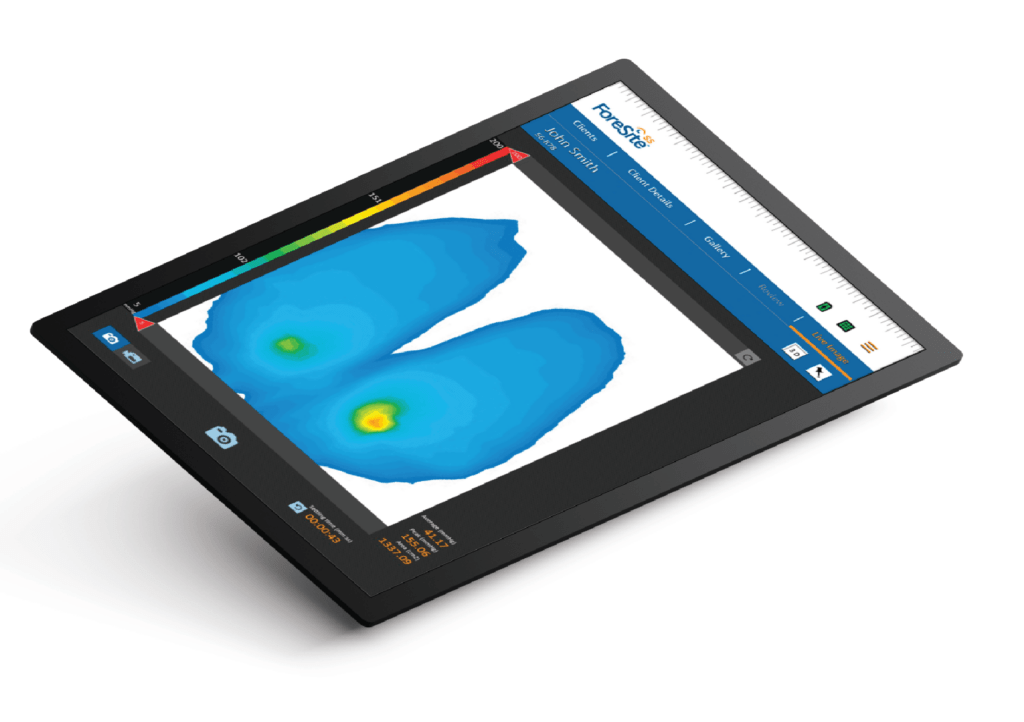
Pressure mapping image of a person sitting in a chair.
Learn more about advanced pressure care solutions
Wider Care Strategies for Healthcare Ulcer Prevention
Pressure strategies can be employed at a wider, more holistic level, to mitigate some of the situations that lead to an increase in pressure wounds generally. These strategies may be harder to implement as they involve greater organisational change, but will reap dividends in reduced wound care costs if implemented effectively.
Early Mobilisation
Mobilising the patient as early as possible in their recovery programme is key to preventing some of the classic causes of pressure wounds. Bed blocking (or ‘pyjama paralysis’ as it is colloquially known in hospitals) leads to patient deconditioning, a process where the muscle mass and physical strength of the patient starts to decline from a prolonged period of inactivity.
Bed blocking happens when patients who are medically fit to be discharged are still occupying hospital beds. This is caused by a variety of factors, covered in more detail in this article. There has been a 12% increase in bed blocking during the 22/23 winter period over 21/22, which will lead inexorably to an increase in deconditioning and resulting pressure sores.
There are a few ways in which bed blocking can lead to pressure problems:
• With older patients, their skin can be thinner and more fragile, making them more susceptible to pressure wounds by lying in a static position
• Immobility can lead to increased incontinence, as patients get out of their toileting routine and rely on incontinence products more. The increase in moisture affects the skin, causing it to break down more easily.
• The speed at which wounds heal, either existing pressure wounds or surgical site wounds, is an important factor. The physical condition of the patient affects this; obesity or poor diet leads to poorer skin health from malnutrition, causing delays in wound healing.
• Long waits for elective surgery can lead to prolonged bedrest, and there is a risk of surgical site infections after operative surgery if the skin is not cared for properly.
The impact of bed blocking on the healthcare system is profound; total wound care costs for the NHS are an astonishing £8.3bn annually. Leg ulcers and diabetic foot ulcers are the most common forms of pressure wound from prolonged bedrest.
Preventing Long Lies
Pressure wounds are just one of the many dangers to someone’s health from a long wait for assistance following a fall (long lie). This risk becomes present after someone has been on the floor for longer than 1 hour in one position, as the sustained loading on their skin can cause pressure injuries to form.

Strategies to improve falls response times are now more critical than ever, with ambulance wait times still high despite having seen a slight improvement.
First responder units and care homes are turning to falls lifting equipment to get fallers to their feet quickly and safely. These are invaluable items of equipment, particularly during winter periods of high demand.
This article covers different strategies to prevent long lies and keep potential fallers safe this winter.
Summary
Policy changes at a higher organisational level can help reduce some of the endemic issues like bed blocking that lead to a greater prevalence of pressure wounds.
Ultimately, pressure care is everyone’s business, and there is no greater substitute for avoiding pressure wounds than high standards of personal care and using the right equipment.
FAQs
Who is most at risk of developing pressure ulcers?
Individuals who are immobile, bed-bound, or confined to a chair for extended periods are at the highest risk. Elderly patients, people with chronic conditions such as diabetes, and individuals with reduced sensory perception are also at increased risk for pressure ulcers.
How can pressure ulcers be prevented?
Pressure ulcers can be prevented through a combination of strategies, including:
• Regular repositioning to relieve pressure
• Using pressure-relieving surfaces such as specialised mattresses or chairs
• Ensuring proper skin care by keeping the skin clean and dry
• Conducting risk assessments using tools like the Braden Scale
• Encouraging early mobility to prevent prolonged immobility
What is the Braden Scale, and how is it used in pressure ulcer prevention?
The Braden Scale is a widely used risk assessment tool that helps healthcare professionals evaluate a patient’s risk of developing pressure ulcers. It assesses factors like sensory perception, moisture, activity, mobility, nutrition, and friction/shear, giving a total score that indicates the level of risk. A score of 16 or lower indicates an increased risk of pressure ulcers.
How does early mobilisation help prevent pressure ulcers?
Early mobility prevents pressure ulcers by reducing the time patients spend in one position, which is a key factor in ulcer formation. Mobilising patients soon after surgery or illness can also prevent muscle deconditioning and improve overall circulation, reducing pressure on vulnerable areas of the body.
How can healthcare organisations reduce the prevalence of pressure ulcers?
Healthcare organisations can reduce pressure ulcers by implementing systemic changes such as improving patient mobility protocols, reducing bed blocking, training staff on proper skin care and repositioning techniques, and using advanced equipment like pressure-relieving chairs and beds. Effective policy changes and the integration of person-centered care strategies are key to reducing ulcer incidence.