Around a third of people aged 65+ fall at least once a year. This figure is even higher for people aged 85+. Many of these older people live in care homes, where there is often a ‘No Lift’ policy.
A ‘No Lift’ policy is designed to protect both the staff and residents against injury. Risk assessments often judge falls as too risky for staff to handle alone. So, the ‘No Lift’ policy becomes part of the wider Health and Safety policy for the care home.
Unfortunately, this means residents are left in an undignified and uncomfortable position until help arrives. UK Ambulance Services are in high demand. So, responding to a fall can take several hours.
What can care homes do about this? How should they manage falls to protect residents, staff, and NHS services?
In this guide, we’ll cover the different assessment tools and emergency equipment care homes can use to respond to falls in the best possible way.
Jump straight to…
What are the risks of remaining on the floor after a fall?
Before we get started, it’s important to remember why managing falls properly is so important for care homes.
Being left on the floor, for any length of time, isn’t good for many reasons.
For older people, a fall can be a major hit to their confidence. Being left vulnerable on the floor can cause lasting damage to their mental health.
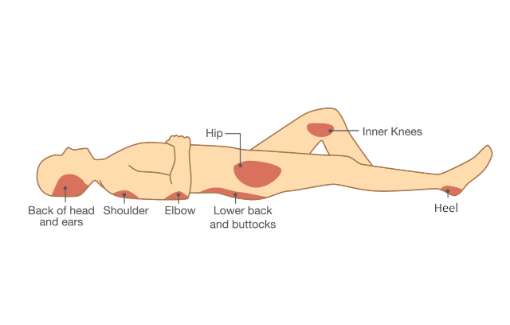
A range of health complications can also develop, including:
- Pressure sores
- Carpet burns
- Dehydration
- Hypothermia etc.
In a care home, a member of staff must always stay with the fallen resident. This is important for keeping them feeling as calm as possible until the ambulance arrives. However, it also means there is one fewer staff to care for other residents.
Assessing for injuries after a fall
The first thing staff must do after a fall is to assess the resident for injuries.
As falls are such a large and common problem, the NHS created a falls assessment tool called I STUMBLE. This is widely used by care homes when responding to a fall.
What is I STUMBLE?
The name, I STUMBLE, is an acronym representing the eight key areas staff should check when a resident falls.
It helps them determine whether there are any serious injuries and decide how best to treat the fallen person.
Before starting the I STUMBLE assessment, always perform the basic first aid checks:
- Is the area clear of dangers?
- Is the resident responding?
- Is their airway open?
- Are they breathing adequately?
- Do they have a pulse?
If the answer is ‘yes’ to these 5 points, proceed to the I STUMBLE fall assessment…
I — Intense Pain
- Is there any new pain since the fall occurred? (E.g. headaches, chest pain and abdominal pain)
- Is the pain caused by the injury or by medical causes?
S — Suspected Collapse
- Ask the resident if this was a trip or collapse? (I.e. Do they remember falling?)
- Did they have any sudden nausea, dizziness, or pain before they fell?
T — Trauma, to Head/Neck/Back
- Do they have any new pain in their head, back or neck following the fall?
- Can you see a visible injury? (E.g. lumps or dents to the head)
- If yes, is it bleeding?
- Does the resident have any new numbness or paralysis in their limbs or face?
U — Unusual Behaviour
- Is there any new confusion to the resident?
- Is the resident acting differently to their normal selves? (E.g. agitated, combative, aggressive, sleepy, or quiet)
- Do they have new difficulties speaking? (E.g. slurred speech, unable to verbalise objects, words mixed up, or stuttering.)
M — Marked Difficulty in Breathing/Chest Pain
- Does the resident have severe shortness of breath? (Initially, they may be in shock. Are they still having breathing difficulties when anxiety is reduced?)
- Are they unable to complete full sentences?
- Are their lips/fingers blue or pale?
- Are they lethargic or confused?
- Do they a new inability to mobilise or lay still without difficulty in their breathing?
B — Bleeding Freely
- Is the blood free-flowing, pumping, or squirting from any wounds?
- Is their widespread swelling and/or bruising?
Tip: Try to ‘estimate’ the blood loss in ‘mug-fulls’. This can help when advising paramedics. Then, apply constant and direct pressure with a clean dressing. Finally, elevate if possible.
L — Loss of Consciousness
- Is the resident knocked out and/or drifting in and out of consciousness?
- Does the resident have limited memory of the events leading up to, during or after the fall? (Where the resident does not have existing memory impairments.)
- Is the resident unable to recall or retain information? (Where the resident does not have existing memory impairments.)
- Is the resident speaking repetitively? (Where the resident does not have existing memory/speech impairments.)
E — Evidence of Fracture
- Is there any obvious deformities? (E.g. Shortened or rotated limb, visible bone, or severe swelling)
- Does the resident have a reduced range of movement?
- Is there any unusual movement?
IMPORTANT: If any of I STUMBLE criteria apply, you must call 999. This indicates the resident has a potentially serious injury and requires emergency medical attention.
What are the benefits of using I STUMBLE?
There are three key benefits of using I STUMBLE in care homes
- When an ambulance is needed, it helps with prioritisation
Ambulance crews are under a lot of pressure. They receive far more calls than they can respond to each day. So, falls without injury are not a priority.
By using I STUMBLE, it means emergency cases can be prioritised. Care home staff can give the call handler an accurate idea of how serious the situation is. Then, an ambulance can attend to provide the required care and take the resident to hospital.
2. It helps avoid unnecessary ambulance callouts
If the I STUMBLE assessment shows the resident is uninjured, staff can consider other options.
Reducing non-emergency callouts could save the NHS millions of pounds per year. Plus, it spares elderly residents an unnecessary trip to hospital. Reducing hospital stays has become a bigger priority for care homes following the COVID-19 pandemic!
3. It gives staff a simple procedure for responding to falls
A fall is stressful for everyone. So having a clear and easy tool to support staff responses is extremely helpful. It takes the pressure off remembering all the checks and allows them to focus on the resident’s wellbeing.
It is very similar to the FAST assessment tool that is well known for determining whether someone has suffered a stroke.
FAST is another good tool to use after a fall
The similarities don’t end at the names… FAST is often used alongside I STUMBLE when assessing someone after a fall:
Face — Is the residents face equal on both sides?
Arms — Is the resident able to hold both arms up without any assistance?
Speech — Is the resident speaking as normal? Any slurring?
Time — Can you get an accurate time of symptom onset?
FAST is something care staff should check after the I STUMBLE assessment to rule out a Stroke as the cause of the residences fall.
What to do if the resident is uninjured?
Falls are a leading cause of hospital admissions in older people. However,
However, many care homes are reluctant to do this, due to their ‘No Lift’ policies.
So, we come back to the issue of residents being left on the floor to wait — despite not needing an ambulance or hospital admission. But this doesn’t necessarily need to be the case.
Do you have a ‘No Lift’ policy?
If you have a ‘No Lift’ policy, there are solutions available.
The ‘No Lift’ policy calls for staff to avoid manual lifting of residents to decrease the likelihood of injury.
However, there are emergency lifting devices available that don’t require any manual lifting!
‘No lift’ fall assist devices
We recommend the Raizer Falls Emergency Lifting Chair. The unique lifting device requires one carer to operate and help a fallen person back to their feet in under 3 minutes.
There’s no manual lifting — electric motors do all the heavy lifting for you. The rising action is gentle and steady to avoid distress and discomfort. Plus, it carries out up to 100 lifts on a single charge. So, it’s ideal for care homes that experience high fall numbers.
I STUMBLE is a quick and effective assessment tool. It allows care staff to work out the seriousness of the resident’s fall and to assess whether an ambulance is needed. Combining this tool with appropriate lifting equipment, like the Raizer, is an effective way to manage falls in care homes.
If you’d like to see the Raizer for yourself, please get in touch. We’d be happy to provide a free demo at your care home or via video call.